Headaches, A Common Malady
A common problem many people experience from time-to-time is a headache. We can still function through the day with a mild headache but they can sometime become so severe as to incapacitate a person. There are many known causes of headaches but there are only a few that occur quite commonly and I believe the classic migraine headache not be among the common causes.
Many patients as well as health care providers will haphazardly use the phrase ‘migraine headache’ when what they really mean to say is “a very painful headache’. The phrase migraine headache should be reserved for a specific cause of headache that is caused by abnormal blood vessel function within the skull and is treated with very specific medication.
Although your headache may be incapacitating, cause you to vomit, see a colorful halo and cause pain one side of the head, it doesn’t at all imply your headache is due to a migraine headache. For instance, sinus headaches can result in incapacitating pain, visual changes and vomiting just as migraine headaches can.
I don’t blame patients for the misuse of the phrase ‘migraine headache’ but I do blame physicians and nurse practitioners for throwing the phrase around without any precision. Its my experience that many health care providers don’t even seem to understand the difference between the different symptom patterns associated with the different causes of headaches.
Other Causes of Severe Headaches
I probably have undiagnosed migraine headaches 10 times more often than I make the diagnosis. Why do I feel that I am correct in changing the patient’s diagnosis? Well, to start with, the patient’s will tell me the wide variety of migraine headache medications don’t help much at all.
Secondly, patients frequently report that the primary health care provider or neurologist haven’t even asked questions about the patient’s allergies, symptoms of lightheadedness, arthritis or muscular tension; clues as to the possible alternative diagnosis of their headaches.
And finally when I carefully asked the patients about the pattern, intensity and timing of their headache pain, what may make it better or worse, the patients will provide me with information that clearly points me away from the diagnosis of migraine headaches and towards a much more likely cause of their pain.
The Most Common Type of Headaches Happen Most Commonly
As the title of this subsection suggests, the most common medical conditions happen most commonly. This may sound simple and commonsensical but believe me, this adage is lost on many health care providers. It’s quite simply the key starting point to solving many of life’s puzzles.
In spite of the lists of causes of headaches that are available on the Internet, few give the reader any sense of which is more common than others. Even those that do try to provide some sense of frequency, they don’t seem to fit my practical observations.
What follows is my practical list of the causes of severe headaches from my perspective as a primary care physician with over 20 years of experience. The list below is what I commonly start from when diagnosing severe headaches:
- Muscle Tension Headaches
- Sinus Congestion Headaches
- Orthostatic Hypotension Headaches
This list helps guide me to correct diagnosis in about 80-90% of my patients with severe headaches. Hopefully some of my following pointers will help you understand the cause of your headache as well.
Muscle Tension Headaches
Muscle tension headaches are extremely common and often cause pain in the temple region of your skull and occur from clenching your teeth (people often do this when they are experiencing lots of stress). Occasionally muscle tension can cause pain at the back portion of the skull called the occiput (usually from muscle tension in the mid to lower back). This is where the muscles from the back and neck attach to the skull. It is also where the muscles that run from the forehead, across of the top of the skull and finally attaches to the back portion of the skull. This pain can be confused with “coat-hanger pain” from orthostatic hypotension (see below).
Patients with muscle tension headaches will often present with pain that starts at the base of the skull and will then radiate forward across the top of the head. The area in a line at the bottom rear portion of the skull is often very tender. Sometimes, it can seem as if the pain is only on one side of the head and this is how it gets confused with classic migraine headaches.
Chronic muscle tension arising from stress, spasm or strain in the upper or lower back often triggers muscle tension headaches. Underlying arthritis in the spine might also trigger this kind of pain.
Another pattern of muscle tension headache is pain that seems to start primarily on both sides of the temples. Most people don’t realize it but this area is where the jaw muscles attach to the skull. Chronic tensing or clenching of the jaw muscles from psychological stress or grinding of teeth while asleep can cause this area of the skull to hurt.
Treating muscle tension headaches involves helping the patients alleviate the source of the muscle tension. Discussions about psychological stressors, back injuries, posture and possible evaluation for dental guards to minimize nighttime clenching and grind are very helpful for these patients.
Sinus Congestion
Your sinuses are small air cavities encased I the bone of your skull that have narrow openings to the nasal passage. They are mostly located in your forehead, behind, between or beneath the eyes. if these narrow openings become congested from allergies, infection or other irritation, the tissue lining the openings swells causing the opening itself to completely blocked. Pain starts developing after blockage occurs.
The tissue that lines the inside of the sinus cavity constantly absorbs small amounts of gas. So when the opening to the sinus is blocked but the tissue continues absorbing gas from within that blocked sinus, a vacuum begins developing within the sinus cavity. The increasing negative pressure from the vacuum is the source of the sinus pain. So the key to resolving the headache is to open the passage and alleviate the pressure.
Pain from sinus headaches can be mild if the sinus is only blocked intermittently or can build to a severe level of pain that includes vomiting, near blindness, color aura, one-sided pain. Sinus headaches may occur intermittently throughout the year but often have a pattern of occurring more commonly during one particular season (Fall more than Spring).
Seasonal fluctuation is the big hint that the mucosal and sinus congestion associated with seasonal allergies are playing a role in the blockage and subsequent vacuum pain of the sinus. Short-term use of decongestants such as Afrin or Sudafed often can lessen the pain of sinus headaches by opening the passage, temporarily relieving the vacuum within the sinus.
Sinus headaches are sometimes associated with occasional sinus infections as well. Sinus infections occur as a result of poor sinus drainage due to an anatomically narrow sinus opening, chronic or severe allergies or an anatomical abnormality such as a deviated septum blocking the sinus opening.
A seasonal pattern of headache, partial or short-term relief with decongestants or intermittent sinus infections is the key to diagnosing severe headaches as coming from the sinuses.
Treatment for this kind of headache often revolves around persistent use of allergy medication such as antihistamines and/or nasal steroid sprays. These treatments limit the swelling of the tissue lining the nasal opening and hence, limit the frequency and duration in which the sinuses may ever become blocked.
Sometime minor sinus surgery is required to repair the underlying anatomical obstruction to the sinus and in my experience, this frequently leads to complete cessation of the sinus headaches.
Orthostatic Hypotension
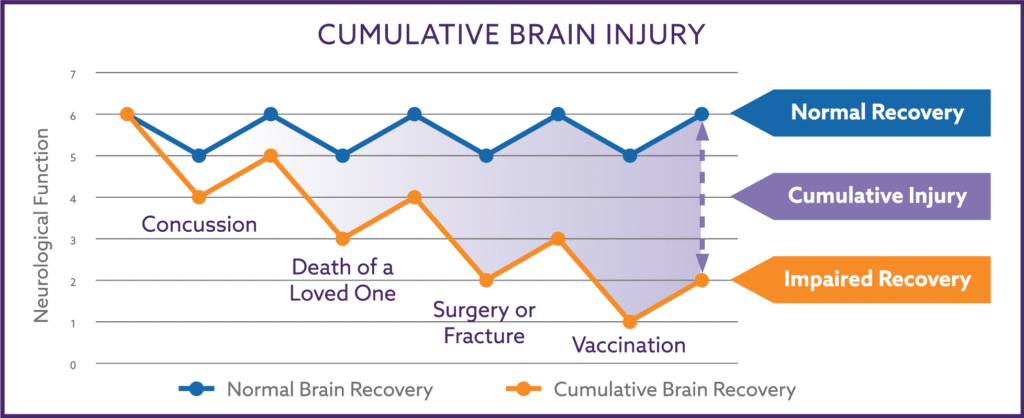
As I have previously discussed, orthostatic hypotension (OH) is a common condition associated with poor perfusion of the brain. OH is associated with occasional lightheadedness, intermittent or chronic fatigue, poor concentration and mild to severe headaches.
OH has many causes but one of the most common is the detrimental effect excessive consumption of carbohydrates (sugar and starch) has on our autonomic nervous system. Excessive dietary carbohydrates are now recognized as the driving force behind the metabolic abnormality known as insulin resistance and it is the development of insulin resistance that is damaging the autonomic nervous system.
OH is also a very common cause of mild to severe headaches. These headaches are the result of inadequate perfusion of blood flow through the brain. As such, they can seem worse after sitting or standing for long periods of time, after eating or after becoming warm or hot. Sometimes they are associated with intense pain in the neck muscles known as coat-hanger pain.
OH headaches are more likely to improve when lying down than other forms of headaches. This because laying flat lessens the pull of gravity that contributes to the low brain blood perfusion. Laying flat makes it easier for your body to pump adequate amounts of blood to your brain; better blood flow means less headache pain because the muscles of the neck and scalp receive better blood flow.
So the big hints for OH as a cause of headaches are:
- Occasional lightheadedness or “woozy” spells just after standing up.
- Fatigue after meals especially bigger meals or high carbohydrate meals.
- Occasional fatigue, poor mental functioning, poor memory or confusion.
- The association of intense neck muscle pain.
Often times symptoms can improve, albeit temporarily, when exercising. This is because constriction of muscles during exercises helps pump more blood from the muscles themselves into the circulation thereby increasing the blood flow to the brain.
OH can get substantially better after increasing the amount of salt and decreasing the carbohydrate intake in your diet. Salt increases your blood volume and makes it easier to maintain adequate blood flow o the brain. The reduced carbohydrate intake allows your autonomic nervous system to recover and more properly control blood flow to the brain.
Think about your headache pain. Does it occur more in one time of the year over another (Fall vs. Spring)? Do you seem to get sinus infections more commonly than your friends or family? Does the pain start in the back of the head or at the temples? Or do you also wrestle with chronic fatigue, have intermittent lightheadedness or intense neck muscle pain?
If you answered yes to any of these, you may need to rethink your diagnosis of “migraine headaches”.
A Simple Test for Orthostatic Headaches
A simple way to check to see if your headaches and other symptoms are from low blood pressure to the brain is to increase the blood pressure to the brain. You can do this simply by increasing the salt in your diet. Salt has a magical property called osmotic pressure that pulls fluid into the blood vessels.
More fluid in blood vessels makes it easier for your heart and blood vessels to provide the proper amount of pressure and blood flow to the brain. Proper blood flow to the brain will allow the brain to function better and should result in a decrease or disappearance of your symptoms if they are due to poor blood flow.
With all the talk by the health officials about the necessity of eating a low salt (sodium) diet, you might be concerned with increasing your salt intake. Don’t worry, its not dangerous for a few weeks. Only person’s with uncontrolled blood pressure, heart failure or kidney disease should talk with their physician before adding salt to there diet.
Follow these instructions to see if your headaches are from low blood flow to the brain:
- Purchase several cans of chicken stock from the market. Chicken stock is full of salt (otherwise known as sodium). Be sure not to buy the “Low Sodium” brands.
- Drink a cup of chicken stock (heat it up a little to improve the taste) in the morning and around midday. This will give you body enough extra blood volume to improve the blood flow to your brain.
- If you find you are fatigued or sleepy shortly after dinner, you may want to have an additional cup then too or even with dinner.
- Within a few days you should notice a significant improvement in your symptoms and your headaches should completely disappear. Remember some people still might have minor headache on occasion from other non-blood pressure related symptoms (e.g., allergies).
Hopefully this simple test helped improve your symptoms. If it did, read the next section about how help your nervous system’s blood pressure regulation system to recover and be able to provide your brain with proper blood flow without need the extra salt.
If it didn’t help at all, you symptoms are probably from a different form of headache.
How to Repair Your Blood Pressure System
If your headaches and other symptoms improved after adding the salt to your diet, you’ll now need to repair the neurological blood pressure mechanism to your brain. This is done by reducing the amount of carbohydrates your consume on a daily basis. Follow these instructions:
- Continue drinking the chicken broth for about 2-3 more weeks after you have reduced the carbohydrates in your diet (see following points). You can switch to other salty foods instead of drinking only chicken stock over these few weeks. Tomato juice has a lot of salt (sodium) in it as do pickles, salsa, sardines, Greek olives and beef broth. Some patients will pour about a 1/4 teaspoon of salt in the palm of their hand and swallow it plain along with some water to wash it down. For convenience, some patients will take a Top Ramen oriental noodle cup (any brand will do) to work and drink only the broth from it.
- Reduce your carbohydrate intake to less than 100 grams per day. It seems switching to higher fiber carbs such as whole grain breads, brown rice or fruit doesn’t help your blood pressure mechanism to repair itself if your total carb intake is still above 100 grams per day. You need to get the total carb count down.
- Some patients find it easier to view their carbs as an allowance. They will save their “carb allowance of 100 grams” for dinner which they find as the most important psychological meal for them. This way they can still have a little rice, pasta or potatoes with dinner and still be under 100 grams per day. You’ll need to read your package labels to get a general sense of how many carbs are contained in some of the common foods you eat.
- Within a few weeks, you will be able to stop the added salt because your blood pressure mechanism will of completely recovered. You headaches and other symptoms should be gone for the most part without the need of the added salt in your diet.
- If your carbohydrate intake increases after recovering neurological blood pressure function, your symptoms will often return rather quickly. You will probably need to change your eating habits permanently if you want to continue to feel this healthy.
- Your symptoms may also return somewhat if your are under a lot of psychological stress, excessively warm or are sitting or standing for prolonger periods of time (such as driving in a car). All of these stressors are known to stress the blood pressure regulatory system.
I hope you have found this information useful. And good luck in your new life free from headaches and the fatigue and clouded thinking that often accompanies them.
Click here to subscribe to Dr. N’s Health Through Nutrition Blog
[/spb_text_block] [spb_blank_spacer2 heightxs=”10″ heightsm=”10″ heightmd=”10″ heightlg=”10″ width=”1/6″ el_position=”last”] [/spb_row]