Over the past year, I have seen many patients with chronic symptoms that began or worsened since being ill with COVID-19 (SARS-Co-V-2 infection). The chronic health issues following COVID-19 are wide-ranging, and 75% of individuals with chronic post-COVID symptoms were not hospitalized during the acute phase of their illness. Those with damaged hearts, lungs or kidneys, or recurrent blood clots are often managed by experts in those fields.
Like many of my adult patients before the pandemic, the individuals seeking my assistance have previously been seen by various other specialists who could not find the cause of their symptoms or have no effective treatment. Unfortunately, most physicians overlook vagus nerve function, autonomic nervous system injury (dysautonomia), bacterial overgrowth, and the potential for recovery from brain injury. Therefore, I feel it is important to share what I have learned about the treatment of post-COVID long haulers.
Lessons from Long Haulers
The short answer is that all the long haulers I have consulted with have significant vagus nerve dysfunction and bacterial overgrowth of their small intestines (SIBO). They often experience many symptoms from inflammatory and direct viral damage to their autonomic nervous system. Treatment with rifaximin (Xifaxan), fish oil, olive oil, and transcutaneous vagus nerve stimulation can dramatically improve their symptoms within just a few months. The components of the protocol collectively lower inflammation, allowing the nervous system to recover and symptoms to resolve.
In addition, many patients have a lingering cough, which everyone presumes from COVID-related lung damage. While SARS-CoV-2 infection certainly causes both direct and indirect damage to the lungs, the post-COVID long haulers I’ve cared for often have a lingering cough which turns out to be from simple postnasal drainage, which usually resolves with 1-2 weeks of twice-daily fluticasone (Flonase) nasal spray.
Treatment of Long Haulers without End Organ Damage
- Single or Repeated Courses of Rifaximin to Reverse SIBO
- Fish Oil and Olive Oil to Lower Inflammation via Omega3:6 Balancing
- Vagus Nerve Stimulation to Regulate Immune Response, Lower Inflammation, and Improve End-Organ Function
- Fluticasone Nasal Spray for Chronic Cough
The following is a more detailed overview discussing the clinical implications of vagus nerve damage, small intestine bacterial overgrowth, inflammatory injury, and autonomic nervous system dysfunction in long-term COVID patients.
A video version of this article is available here.
Vagus Nerve Injury and Associated Symptoms
The vagus nerve is the unique nerve of the human body. All nerves that extend from the central nervous system function similarly to a single insulated copper wire one might think of in their home. The vagus nerve is different; it is composed of 60,000 insulated wires, and 80% of the electrical signaling carried in the nerve travels not from the brain down (efferent signaling) to the body but from the body upwards to the brain (afferent signaling).
In a certain respect, just as the spinal cord is understood to be a complicated bundle of neurological “wires” or nerves, the vagus nerve can be thought of as a small spinal cord with complex bundles of “wires” running down either side of the neck.
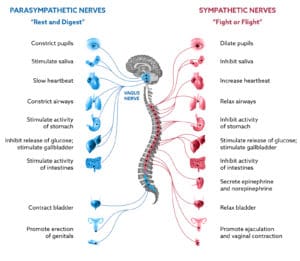
The vagus nerve carries signals from the parasympathetic branch of the autonomic nervous system and influences the function of all body organs, including the immune system. If the vagus nerve does not function properly, many symptoms can occur because the body does not function properly.
List of Symptoms Attributable to Vagus Nerve Dysfunction
- Inflammatory Pain
- Chronic Fatigue
- Poor Focus, Impaired Memory
- Constipation
- Reflux, Heartburn, Bloating
- Nausea, Decreased Appetite
- Rapid Heart Rate
- Dizziness or Lightheadedness
- Trouble Swallowing, Food Sticking in Esophagus
- Altered Voice
- Shortness of Breath (“Air Hunger”)
- Anxiety, Panic
- Difficulty Falling Asleep
- Headaches, Neck Tightness
Due to its numerous branches, the vagus nerve has the highest surface area of any nerve in the human body. Unfortunately, the large surface area causes the nerve to be susceptible to toxic substances within the bloodstream. The vagus nerve will not function properly when exposed to excessive blood sugar, chemotherapy, or inflammatory cytokines such as those released during Sars-CoV-2 infection.
Recent studies illustrate the extent of vagus nerve dysfunction in patients recovering from COVID-19. A recent pilot trial examined the vagus nerve with ultrasound and demonstrated thickening of the vagus nerve and increased ‘echogenicity,’ which indicates mild inflammatory reactive changes. The same report estimates that 86% of COVID patients with chronic symptoms have three or more symptoms associated with chronic vagus nerve dysfunction. These symptoms were present for a median of 14 months when the subjects were evaluated.
Another critical effect of vagus nerve injury and dysfunction is that the inflammatory response to infections and injury is not regulated correctly, leading to chronic inflammation. Chronic inflammation is the primary mechanism preventing nervous system damage symptoms from resolving.
Small Intestine Bacterial Overgrowth is a Consequence of SARS-CoV-2 Infection
Long-hauler COVID-19 patients commonly experience gastrointestinal symptoms such as bloating, heartburn, reflux, abdominal cramping, occasional loose stool, and some stool urgency after eating. Without any other cause, such as inflammatory bowel disease or concerns about chronic pathogenic infection (salmonella, giardia, etc.), these symptoms are highly suggestive of SIBO. From my experience treating thousands of such patients, I believe many long-hauler COVID patients are experiencing gastrointestinal and non-gastrointestinal symptoms resulting from small intestine bacterial overgrowth (SIBO).
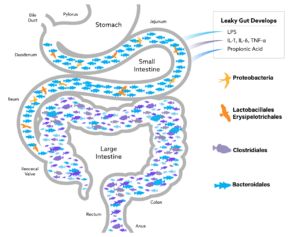
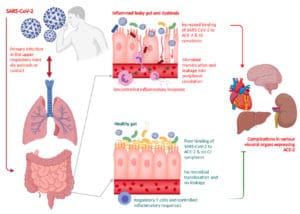
SIBO is an overgrowth of bacteria within the small intestine. The bacteria overgrowing the small intestine are species commonly originating from the large intestine (colon). Overgrowth is a significant cause of chronic inflammatory bacterial translocation, widely called “leaky gut” (figs. 1 & 2).
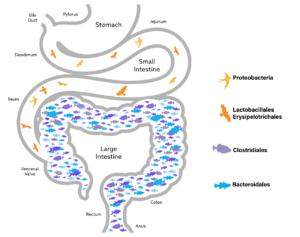
A common trigger for the development of SIBO is a significant decrease in the natural motility of the small intestine. General anesthesia, abdominal surgeries (bowel and gastric resection, cholecystectomy, hysterectomy), brain injury (concussions, major brain trauma), chemical injury (chemotherapy, propionic acid, chronic elevation of blood sugar), and certain medical conditions (chronic renal failure, scleroderma) are all associated decreased small intestine motility and increased rates of SIBO.
Since early in the pandemic, various studies have illustrated how SARS-CoV-2 infection disrupts the normal balance of colonic intestinal bacteria (dysbiosis). SARS-CoV-2 also causes direct neurological injury to the small intestine resulting in slowed motility and the development of SIBO.
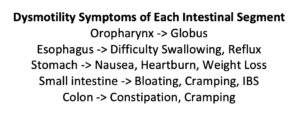
In essence, each segment of the intestinal tract is a segment of the entire gastrointestinal conveyor belt, with each component causing unusual symptoms or conditions if the motility of that intestinal segment slows.
The small intestine neurological injury is possibly related to the ACE2 receptors critical for the SARS-CoV-2 virus to attach and infect human cells. The small intestine has the largest known concentration of ACE2 receptors in the human body. After SARS-CoV-2 binds to the ACE2 receptor, the virus can enter the cell, disrupt cellular function, and even result in cell death.
The cellular stress from SARS-CoV-2 infection leads to a breakdown in the small intestine’s protective barrier resulting in bacterial translocation (leaky gut). COVID-associated bacterial translocation has been reported to contribute to the overriding inflammatory stress (see here, here, and here), which is the primary driver of morbidity and mortality.
Fortunately, the non-absorbable antibiotic rifaximin often dramatically improves symptoms of COVID-associated SIBO.
Inflammation is the Underlying Trigger of Symptoms and Disability in COVID-19
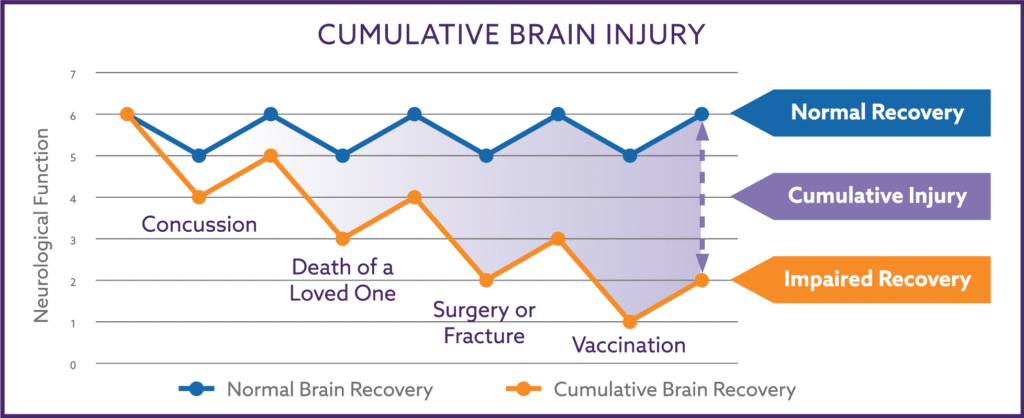
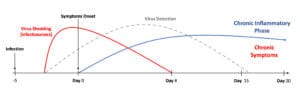
The earliest symptoms of COVID-19 come from the immune response to the virus. Individuals often experience fever, chills, muscle aches, cough, etc., for a few days, and then the symptoms spontaneously resolve as the virus is cleared from the body (red line), as shown in figure 3. The inflammatory phase (blue line) also subsides and reaches baseline as the symptoms resolve. Fortunately, most individuals with symptomatic infection have only mild-to-moderate symptoms which completely resolve.
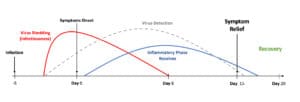
Unfortunately, about a third of those infected with SARS-CoV-2 but who were not hospitalized report chronic symptoms and a deterioration of their health one year after infection, as shown in figure 4. COVID patients with chronic symptoms also have a prolonged state of immunological stimulation (blue line) eight or more months after infection. These patients often have a wide array of symptoms, with gastrointestinal problems prominent among them.
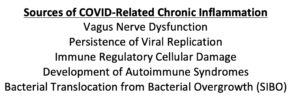
The chronic inflammation seen in COVID long haulers is the cumulative inflammatory burden from new and pre-existing inflammatory stimuli.
Pre-existing sources of inflammation are varied and much more common than most clinicians are aware of (fig. 5).
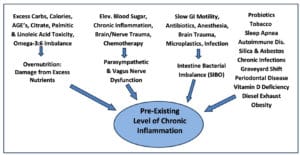
New sources of post-COVID inflammation include persistence of viral replication, underlying vagus nerve damage, immune system regulatory mechanisms, triggering of autoimmunity syndromes, and development of bacterial translocation from bacterial overgrowth (SIBO).
As one can see from the preceding figure, my approach is to extinguish the excessive inflammatory stress coming from three primary sources: overnutrition, vagus nerve dysfunction, and the imbalance of intestinal bacteria. The right column is a variety of less common but potentially significant sources of inflammation that also need to be considered.
Reducing Inflammation Due to Overnutrition
Overnutrition is a term reserved for cellular damage that occurs from the intake of excess nutrients; it does not imply being overweight or obese. An example of overnutrition might be blindness which arises from the excessive intake of vitamin A.
A significant source of inflammatory overnutrition is the excessive amount of dietary omega-6 fatty acids found in vegetable oils and grain-fed livestock. The primary omega-6 fatty acid is linoleic acid, located in high concentrations within margarine, shortenings, and vegetable oils such as soy, corn, safflower, and sunflower. When animals are fed large amounts of corn and soybeans, the linoleic acid within the grains is converted into high concentrations of another inflammatory omega-6 fatty acid, arachidonic acid, which concentrates within livestock meat.
Small amounts of linoleic acid and arachidonic acid are required to normalize a healthy inflammatory response by the immune system. Primitive humans evolved by consuming a 1:1 ratio of omega-6 (inflammatory) and omega-3 (anti-inflammatory) molecules (figure 6). This ratio allows healthy inflammation to occur when needed to fight infections or repair tissue. At the same time, the anti-inflammatory omega-3 fatty acids consumed in fish and shellfish are used to turn off the inflammation appropriately.
Unfortunately, our modern western diet contains excessive omega-6 fatty acids that shift the inflammatory process onto overdrive and lead to chronic inflammation. The large amounts of omega-6 fatty acids in our diet have the effect of consuming cellular gasoline, which leaves the body in a state of chronic inflammation, further damaging tissue and preventing the repair of nervous system damage.
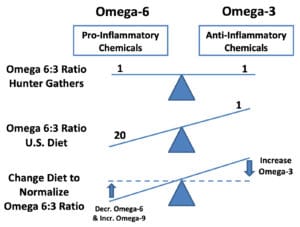
Fortunately, the high concentration of oleic acid (an omega-9 fatty acid) present in extra virgin olive oil fully shields the body from the inflammatory nature of linoleic and arachidonic acids. This protective, anti-inflammatory feature of extra virgin olive oil makes daily consumption of primary importance. The additional consumption of omega-3 fatty acids from fish oil help to heighten the benefit of extra virgin olive oil.
As shown in figure 5, there are additional sources of overnutrition inflammation, such as advanced glycemic endproducts, citrate, and palmitic acid consumption. The reader can find other resources discussing the inflammatory nature of these substances.
My Clinical Experience
For over 20 years, I have been developing The Nemechek Protocol®, a highly effective process for reducing chronic inflammation that often results in profound improvements in neurological function. The Nemechek Protocol® is proven effective and was even issued a U.S. patent for its unique capabilities.
I have found that the core elements of The Nemechek Protocol® are also very effective at helping reduce chronic inflammation and the associated symptoms in post-COVID long haulers.
I empirically treat SIBO without testing for two significant reasons. The first is the commonly used hydrogen-methane breath tests for SIBO are often inaccurate. I have had many patients with dramatic improvements after treatment for SIBO despite a negative breath test indicating SIBO was not present.
The second is that I use rifaximin to treat SIBO, and because this medication is not absorbed within the bloodstream, it is incredibly safe with few to no side effects. The improvement experienced after rifaximin treatment is from reversal damage to the small intestine, reduced inflammation, and improved function of the vagus nerve and autonomic nervous system.
Treatment of SIBO is more than just a one-time eradication of the excessive bacteria within the small intestine, as one might typically think when treating an infection within the bladder or sinuses. Treatment of SIBO involves managing repeated relapses of excessive bacteria growth. Spontaneous relapses usually occur because of underlying neurological damage and dysmotility to the small intestine.
Many patients require repeated courses of rifaximin to control inflammation and prevent their SIBO symptoms from returning. Lower levels of inflammation allow the nervous system motility of the small intestine to recover and enable other symptoms from their underlying autonomic nervous system to resolve.
Although a patient might require several rounds of rifaximin over a year, they become less and less frequent due to the small intestine’s improved nervous system dysfunction and motility.
Autonomic Dysfunction and Restoring Small Intestine Motility
The autonomic nervous system (ANS) is the coordination center of other aspects of your nervous system. Its two branches (sympathetic and parasympathetic) help regulate most parts of your physiology (organs, blood pressure, heart rate, emotions, inflammation, hormones, metabolism) depending on the stress your body is experiencing (figure 8). As one can imagine, your body operates quite differently, whether you are sound asleep or being chased by a tiger. In these different scenarios, your autonomic nervous system is responsible for the various physiological responses (relaxation vs. fear and panic).
The ANS is easily injured after common physical brain injuries such as concussions but can also be damaged after intense emotional traumas (sexual assault, death of a loved one, combat) or surges in inflammation commonly seen in COVID-19.
When injured, the ANS does not function correctly and results in symptoms arising from two distinct physiological problems, reduced blood pressure in the brain and reduced motility of the intestinal tract. The reduced brain blood pressure (cerebral hypoperfusion) results in headaches, neck tightness, brain fog, poor concentration and memory, increased hunger and thirst, anxiety, altered balance, and occasional passing out (syncope).
The reduced motility of the intestinal tract can result in difficulty swallowing, reflux, heartburn, bloating, cramping, and constipation. These are common symptoms experienced by post-COVID long haulers. In addition, slowed intestinal motility increases the risk of SIBO.
Spontaneous relapses of SIBO are common because slow intestinal motility persists even after antibiotic treatment of SIBO. The dysmotility of the small intestine will only improve after the ANS recovers. Suppose ANS recovery does not occur within the first few months after the injury, such as SARS-CoV-2 infection. In that case, it is unlikely to recover unless systemic inflammation is significantly reduced for several months.
If you are wondering if you are experiencing autonomic dysfunction for COVID infection or otherwise, you can take a simple self-test on my practice website. If your score indicates autonomic dysfunction, you have a good chance of significant improvement following my protocol.
Decrease Long-Hauler Symptoms
To reverse the symptoms of nervous system damage and SIBO, the protocol must suppress chronic inflammation by changing bacterial overgrowth, controlling primed-M1-microglia within the brain, rebalancing omega-3 and omega-6 fatty acids, and improving the vagal anti-inflammatory reflex via vagus nerve stimulation and symptoms of autonomic dysfunction in post-COVID long haulers who seek my help.
More details and scientific references about The Nemechek Protocol® can be found in our book on treating autism. I want to apologize to my adult readers that the demand for research and advice on treating autism has prevented me from completing The Nemechek Protocol Guide for Adults but take note that the doses I specify in the book for adults with autism are identical and were initially designed for adults with autonomic dysfunction.
The Nemechek Protocol® Dosing for Adults
- Rifaximin (Xifaxan™️) 550 mg twice daily for ten days; repeat as necessary
- DHA-500 fish oil (NOW Foods), six capsules per day, or 1 tbsp (15 ml) of Nordic Naturals Ultimate Omega liquid fish oil.
- High Phenolic, COOC-Certified Olive Oil (Nemechek Gold™️), two tbsp per day
- Transcutaneous Vagus Nerve Stimulation, 5-120 minutes per day
As mentioned earlier, I use repeated courses of rifaximin to reverse the ill effects of SIBO. The first 10-day course of rifaximin often profoundly improves symptoms of most long-haulers. Because of the dysmotility and neurological injury to the small intestine, most patients will require repeated courses of rifaximin before the SIBO relapses become less frequent.
On occasion, the relapses occur within 1-2 weeks after finishing a course of rifaximin and then I will employ a 4-6 month period of continual, non-stop twice, daily rifaximin. By controlling bacterial overgrowth and the associated inflammation, the small intestine motility improves, and subsequent bacterial relapses become less frequent.
Supplementing fish oil and extra virgin olive oil stabilizes the omega-3 and omega-6 fatty acid balance. These omega-fatty acids are essential in initiating and resolving inflammation within the body. Excessive amounts of omega-6 fatty acids within the food supply encourage the body’s inflammation system to become excessively activated and inhibit the nervous system’s ability to down-regulate (turn off) inflammation. Because of the high rate of substandard products sold in the supplement and olive oil market, I recommend NOW Foods and Nordic Naturals because of their reliability and COOC-certified (California Olive Oil Council) extra virgin olive oil.
Stimulation of the vagus nerve at the ear is referred to as transcutaneous vagus nerve stimulation (taVNS) and can profoundly improve normal inflammation regulation. My group studied the inflammation-controlling impact of taVNS in hospitalized COVID patients and reported the lowest use of mechanical ventilation and second-lowest mortality rates in hospitalized COVID patients requiring supplemental oxygen. The results were convincing enough to be issued a patent (U.S Patent 10,335,396).
Although implantable VNS devices have been available for 20 years, a taVNS device is not readily available through your physician or neurologist. Some stimulation devices used for other indications are available by prescription. In contrast, others are being sold as consumer wellness devices that can mimic the anti-inflammatory effects believed to be responsible for the benefits seen in our study. Patients seen in my office are often prescribed a taVNS device for daily use at home.
Although taVNS is often required daily, the vagus nerve seems to be able to recover enough that VNS ultimately is no longer or only intermittently required.
Case Report
William is a 55-year-old male who came to me after experiencing chronic problems since being mildly symptomatic with COVID in January 2020. He was experiencing a persistent cough and fever that fluctuated in intensity for about six weeks and then developed other symptoms that steadily worsened.
William is a financial consultant for major corporations, frequently traveled to teach large seminars, and rarely ever missed a day of work. But as his illness worsened over the first few months, he missed more work. He began experiencing shortness of breath, intense fatigue, nausea, and lightheadedness. The symptoms fluctuated in intensity over the following months, but by June, he began making critical errors in his consulting work.
By August 2020, his cognitive function had deteriorated to the point that he had trouble completing even the most straightforward task. His fatigue became so intense that he was forced to quit working altogether. Although his intermittent fever and recurrent sinus infections seemed to stop, he was still experiencing frequent headaches, chronic constipation, irritated eyes, shortness of breath and nausea, and rapid bloating, especially when trying to eat. Consequently, he lost 50 pounds and was only a shell of his former physical and intellectual self.
William first saw me in my office in Oct 2020. He was started on The Nemechek Protocol® using intermittent 10-day courses of twice-daily rifaximin, fish oil (DHA-500, NOW Foods, six capsules/d), extra virgin olive oil (Nemechek Gold, two tbsp/d), and two hours of transcutaneous vagus nerve stimulation daily.
He was seen four months later and reported that the intermittent courses of rifaximin led to him feeling much better immediately. He said feeling more focused and energetic, slept better, had less nausea, improved appetite, and had gained 15 pounds.
William said that a few weeks after finishing a round of rifaximin, his symptoms would return but would once again improve after taking another course of rifaximin. Because of the frequency of relapses, he was started on a 4-month course of continuous twice-daily rifaximin and continued daily fish oil and olive oil supplementation and daily vagus nerve stimulation.
By July 2021, he had almost regained almost all his weight, constipation and sleep improved, and cognition and lightheadedness improved. He was shifted from continuous to intermittent rifaximin and continues taking fish oil and olive oil and using his vagus nerve stimulator.
William continues with daily fish oil, olive oil, and vagus nerve stimulation and only requires rifaximin every 3-4 months. His strength and weight have returned, and he has been able to resume working as a financial consultant. Although his symptoms were more severe than most COVID long-haulers I’ve cared for, his level of improvement is quite common among most of the patients I’ve cared for.
Summary
I hope this quick review is helpful to those affected with long COVID symptoms. The rifaximin, fish oil, and olive oil alone are often effective enough to improve your symptoms and are readily available.
The fish oil and olive oil can be easily ordered online, and rifaximin is sold in the U.S. under the tradename Xifaxan and can be prescribed by your physician. If your insurance does not cover Xifaxan, the generic version of rifaximin is readily available through Canadian mail-order pharmacies.
We are in the early stages of seeing other long-term symptoms of COVID-19, and studies have now shown the brain after SARS-CoV-2 infection can prematurely age 20 years. I believe The Nemechek Protocol, which was developed and patented for brain and nervous system injuries and dysfunction, can also help individuals with chronic post-Covid symptoms.