Typical Patient Encounters
37-Year-Old Female with POTS, Fatigue, Anxiety and Long COVID
Going from Mild Symptoms to Incapacitated
Jennifer is a 37-year-old female who was in generally good health until her late 20s, when she began to have intermittent headaches, which at times were severe. Over time her headaches became more frequent, especially after the birth of her second child. She was diagnosed with migraine headaches and prescribed medication to treat the headaches. The after her father unexpectedly passed away from a heart attack, she began feeling unexplainably tired at times, making it difficult to even care for her children. To make matters worse, her anxiety began spiking without reason.
She then contracted what she thought was a relatively mild case of COVID in the Spring of 2022, and her health seemed to shift from difficult to horrible. Many times a day, when she would stand, she would experience a swooning feeling as if she might pass out, and her heart would beat so hard and fast she felt it might explode. Her anxiety increased to full-blown panic attacks, and the painful migraine headaches were occurring almost daily. She felt so bad at times that she was unable to get out of bed for most of the day.
Visits to the emergency room, and her primary care doctor only showed an elevated heart rate when upright. All other testing (blood work, EKG, CT scan of her heart) were always normal. She was finally diagnosed with POTS (postural orthostatic tachycardia syndrome) by a cardiologist after performing a tilt table test. She was treated with medication to control the extreme heart rate (propranolol), but she was still extremely fatigued, frequently lightheaded, suffering frequent headaches, and constantly anxious.
Jennifer’s Symptoms were from Autonomic Dysfunction
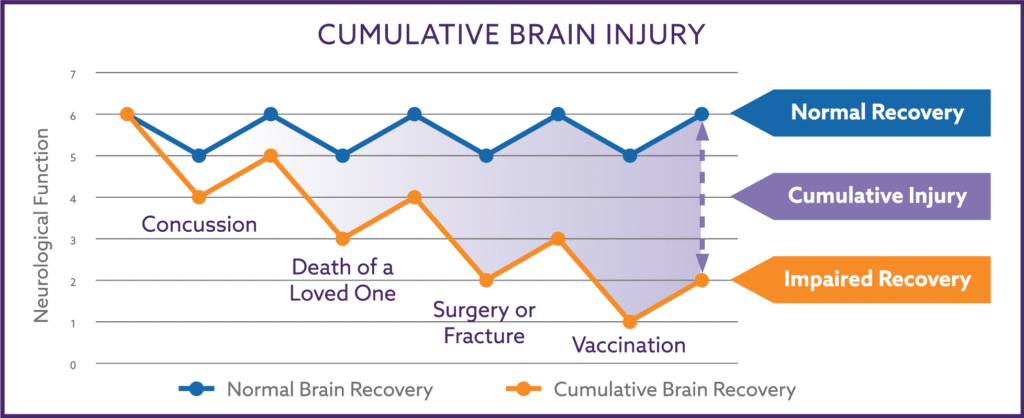
Jennifer’s history is a classic description of symptoms resulting from a damaged and poorly functioning autonomic nervous system (ANS). The ANS is a portion of the central nervous system and regulates a person’s blood pressure, heart rate, all organs of the body, and most other physiological function such as metabolism, immune function, hormone regulation, and emotional regulation. ANS injuries commonly occur from concussive or subconcussive physical, emotional, or inflammatory injuries to the central nervous system. Fortunately, the ANS can fully recover from these injuries within a few weeks to months if the central nervous system is healthy and well-nourished.
Autonomic injuries can occur from emotionally unsettling events, painful hits to the head, or the inflammatory stress from surgery, fractures, vaccines, or infections such as COVID. For most of us, the injury caused by these common injuries will only cause temporary damage, which will be repaired within a few weeks to months after they occur. Unfortunately for Jennifer, her body was experiencing inflammatory stress, preventing her brain’s normal injury repair mechanisms from functioning properly. Consequently, her minor injuries from seeming common events were not fully repaired. The residual damage left behind from each injury increased the cumulative damage of prior injuries resulting in worse and worse functioning of her autonomic nervous system.
Only specific testing of the autonomic nervous system could demonstrate the damage that was causing her symptoms, and, unfortunately, this type of testing is readily available. The tilt table test performed by her cardiologist is an example of autonomic testing. No other X-ray, scan, or blood test can detect autonomic dysfunction. Because of Dr. Nemechek’s clinical and research experience, he can accurately diagnose autonomic dysfunction based upon the absence of abnormalities on standard testing combined with the unique symptoms caused by autonomic damage.
Recovery with The Nemechek Protocol
The principle of The Nemechek Protocol is based upon recent discoveries that the nervous can recover from all but the most devastating brain injuries as long as it is not experiencing abnormally excess levels of inflammatory stress. The inflammatory stress results from an abnormal release of inflammatory chemicals known as cytokines released from activated white blood cells (WBCs). The modern world we have created has inadvertently created a variety of sources of inflammatory stress which, when combined, can trigger a wide range of medical conditions (diabetes, cancer, cardiovascular disease) as well as prevent the central nervous system from recovering from injuries. The Nemechek Protocol focuses on three major sources of excessive inflammatory stress, the overgrowth of bacteria within the small intestine, a relative imbalance of omega-3 and omega-6 fatty acids, and the failure of the Vagus nerve to properly regulate inflammation.
Jennifer was started on a course of the non-absorbable antibiotic rifaximin to reverse and control the overgrowth of bacterial within the small intestine (i.e., SIBO), daily olive oil to block the inflammatory stress from inflammatory omega-6 fatty acid linoleic acid, a high dose of a blend of fish oil designed to penetrate the central nervous system and daily Vagus nerve neuromodulation more readily.
Shortly after starting the regimen, Jennifer noted that some previously disturbing intestinal symptoms quickly stopped, and her anxiety somewhat improved. Over the next 2-3 months, she began noticing occasional days of improved energy and less lightheadedness, and her headaches were occurring less frequently and seemed less intense. By her 6th month on the protocol, she commented to Dr. Nemechek that although she was “completely normal yet”, she was feeling better than she had in many years. She no longer required taking the propranolol, was able to fully care for her children without difficulty, and her panic attacks had completely stopped.
She is now on a daily regimen of fish oil and olive oil and occasional courses of rifaximin whenever she feels the intestinal symptoms from her bacterial overgrowth return. She occasionally will use Vagus nerve neuromodulation to help the more rapid recovery of any subsequent injuries she experiences. She only needed to travel to Dr. Nemechek’s office once during this time to become established as a patient within his practice. Her follow-up visits were done via Skype, and after 12 months, her primary care provider was so impressed with her recovery that they agreed to continue to provide refills of her rifaximin should that be needed.
42-Year-Old Male with Heartburn, Neck Pain, Lightheadedness and Increasingly Worse Focus
A Dramatic Decline in Functioning after the Loss of a Loved One
Dennis is a 42-year-old male who thought of himself as being in generally good shape until the past few years. He exercised regularly, tried not to overeat during business lunches and dinners, stopped smoking in his twenties, and generally only drank alcohol on the weekends. He had experienced mild heartburn over the last 15 years or so but could control it by avoiding eating cooked tomatoes and overly spicy foods.
In the last few years, he began noticing having more trouble when he needed to work on important projects for work. When working on. financial reports for work, he would need to sit for prolonged periods of time. Normally, he could work many hours on end with excellent focus and get a lot of work done. But more and more, he began noticing that after 30-45 minutes, an uncomfortable pain across his neck and shoulders would develop. Additionally, the pain was so aggravating at times it was interfering with his focus and productivity. He discovered the pain would subside quite a bit if he took a break from work and either lay flat for 30 minutes or go for a walk around the block (he worked from home). Although inconvenient, the solution was simple enough, take a break from sitting at his desk every hour or so and work around the block or even exercise a little, then he could work some more. Things took a change for the worse when tragedy struck; Dennis’ brother Michael was killed in an automobile accident.
Dennis and Michael were extremely close, texting each other daily without fail. Quite naturally, the loss of a family member causes a great deal of emotional grief and a great sense of loss, but something else happened to Dennis. From the moment he heard about his brother’s death, he felt so lightheaded that he thought he might pass out. It seemed almost natural at the moment, but what confused him was that even after the immediate shock of Michael’s death had subsided, the lightheaded spells did not stop. Day in, day out, either when standing still too long or getting up from bed or a chair, he would feel like he would pass out. And to make matters worse, his neck pain was now almost constant if he was in an upright position, his focus had deteriorated so much he was falling behind with his financial reporting, and he was beginning to gain weight because he was snacking constantly to control his nausea.
He was evaluated by his primary care physician, a gastroenterologist, a neurologist, and a cardiologist. All the testing he underwent was either normal or inconclusive. He was placed on a PPI antacid which helped lessen the reflux somewhat but didn’t help with his nausea. The neurologist tried him on a few different medications for the poor focus, which he was told was ADD (attention deficit disorder), but these all seemed to increase in anxiety and made it actually harder to think correctly.
Emotional Trauma Caused Autonomic Dysfunction
Dennis’ medical history is a common scenario; marked worsening of autonomic nervous system function because of intense emotional trauma. Emotional trauma is a well-known phenomenon and, in its worse form, known as a takotsubo event, can sometimes be fatal (e.g., “dying of a broken heart”). Prior to Michael’s death, Dennis’ history was indicative of mild autonomic dysfunction from cumulative brain injury because of chronic neuroinflammation, most likely stemming from bacterial translocation (leaky gut) due to small intestine bacterial overgrowth (SIBO).
Whether it be from physical, emotional, or inflammatory insults, brain traumas commonly cause two different mechanical issues, which account for a variety of symptoms. The first is a decrease in blood pressure in the head and neck region. Low blood pressure makes it difficult for red blood cells to release oxygen into the tissues and thereby causes the tissues not to work correctly. If a muscle does get enough oxygen, it causes pain, and this is the cause of Dennis’ neck pain which is often referred to as coat hanger pain. Lack of oxygen released into the scalp muscle is increasingly believed to be the cause of most headaches, including migraine headaches. It also can lead to pain and tightness in the jaw muscles, mimicking the symptoms of TMJ. Lack of oxygen into the brain tissue is the cause of Dennis’ lightheadedness and worsening focus. Poor brain oxygen delivery can also cause altered balance, anxiety, increased hunger, increased thirst, abdominal pain, air hunger, foot tapping, and other fidgety behaviors.
The second mechanical effect of brain injury is that the forward motility action of the intestinal tract slows down. Each segment of the intestinal tract has unique symptoms suggesting its forward propulsion of intestinal contents has slowed. The esophagus will lead to the sticking of both liquids and solids, while decreased stomach motility can trigger nausea, post-meal vomiting, heartburn, and reflux. Slow motility of the small intestine can trigger IBS-like cramping, but many times, there are no direct symptoms, only the frequent occurrence or relapsing of SIBO. And slow motility of the colon leads to constipation.
If the nervous system is functioning properly, the injury that results in any of these symptoms will be fully repaired within a few weeks to months, and the symptoms would completely resolve except for if SIBO was triggered, this would need treatment with rifaximin or another antibiotic regimen to reverse. Unfortunately, Dennis’ symptoms for particular food intolerance is a common sign of leaky gut from SIBO, which commonly results in high levels of systemic and central nervous system (CNS) inflammation as well as priming of M1-microglia white blood cells within the CNS. Both persistent CNS inflammation and M1-microglia priming prevent brain traumas from recovering completely. There were signs of early autonomic damage in Dennis’ history, with the gradual worsening of his neck tightness and pain, which are manifestations of coat hanger pain.
Recovery
The principle of The Nemechek Protocol is based upon recent discoveries that the nervous can recover from all but the most devastating brain injuries as long as it is not experiencing abnormally excess levels of inflammatory stress. The inflammatory stress results from an abnormal release of inflammatory chemicals known as cytokines released from activated white blood cells (WBCs). The modern world we have created has inadvertently created a variety of sources of inflammatory stress which, when combined, can trigger a wide range of medical conditions (diabetes, cancer, cardiovascular disease) as well as prevent the central nervous system from recovering from injuries. The Nemechek Protocol focuses on three major sources of excessive inflammatory stress, the overgrowth of bacteria within the small intestine, a relative imbalance of omega-3 and omega-6 fatty acids, and the failure of the Vagus nerve to properly regulate inflammation.
Dennis was started on a regimen of brain-penetrating fish oil, olive oil, and a short course of rifaximin. Initially, his insurer would not cover the rifaximin, but he was finally able to affordably acquire rifaximin using a Canadian mail-order pharmacy. His intolerance to spices and tomatoes improved while he was on rifaximin but returned within a week or so of completing the 10-day course. This means that the intestinal motility of the small intestine has slowed considerably to such a degree that SIBO is relapsing very quickly once the rifaximin is discontinued. As a consequence of the rapid relapsing, he was started on a continuous course of twice-daily rifaximin.
Over the first few months, Dennis’ intestinal issues and lightheadedness slowly began to improve. He then opted to try Vagus nerve neuromodulation, which resulted in an acceleration of his recovery and had the pleasant effect of reducing his anxiety within minutes of each daily treatment. Dennis’ follow-up visits were performed via Skype every few months, and after seven months, his heartburn, lightheadedness, poor focus, and neck pain were almost completely gone, and he was successfully shifted from continuous to intermittent courses of rifaximin.